The Diagnosis – Facing iSGS
- Lyndsey Paprota

- May 19, 2025
- 6 min read

In my previous post, I shared the early symptoms and initial confusion that marked the beginning of my struggle with Idiopathic Subglottic Stenosis (iSGS). What started as shortness of breath, stridor, and mounting anxiety around my breathing soon became impossible to ignore. With encouragement from my now husband, I finally started seeking medical help—but getting answers would take time, persistence, and a lot of emotional strength.
🛣️ The Road to Diagnosis
My diagnostic journey began on September 22, 2017, when I finally went in for an initial evaluation. I had been experiencing stridor (a high-pitched wheeze) and shortness of breath, especially during exercise, for quite some time — but I ignored it. I was juggling three jobs, fresh out of college, and completely overwhelmed. I kept telling myself I didn’t have time for doctor visits.
My now-husband, however, was the one who noticed the stridor and pushed me to seek help. I finally saw a local ENT, who performed a nasal endoscopy. Initially, they dismissed my symptoms and told me it was likely asthma, even though I felt deep down that something wasn’t right. I had to advocate strongly for myself, returning for multiple visits to push for further testing.
What followed was a cascade of appointments and tests:
ENT evaluation and repeat nasal scoping
Allergy testing
Bloodwork with a naturopath
Referral to a pulmonologist
A thorough autoimmune and inflammatory workup with Dr. Zachary Wallace, a rheumatologist at Massachusetts General Hospital
Dr. Wallace worked to rule out rheumatologic conditions, and because my C-reactive protein (CRP) remained elevated, I underwent two Rituximab infusions, each lasting five hours, to see if reducing systemic inflammation would help with my airway symptoms.
Finally, in early January 2018, I was formally diagnosed with Idiopathic Subglottic Stenosis (iSGS) by Dr. Henning Geisert. Since that time, I’ve been under the care of Dr. Ramon Franco, an otolaryngologist who continues to manage my case and procedures.
🗓️ Procedure Timeline
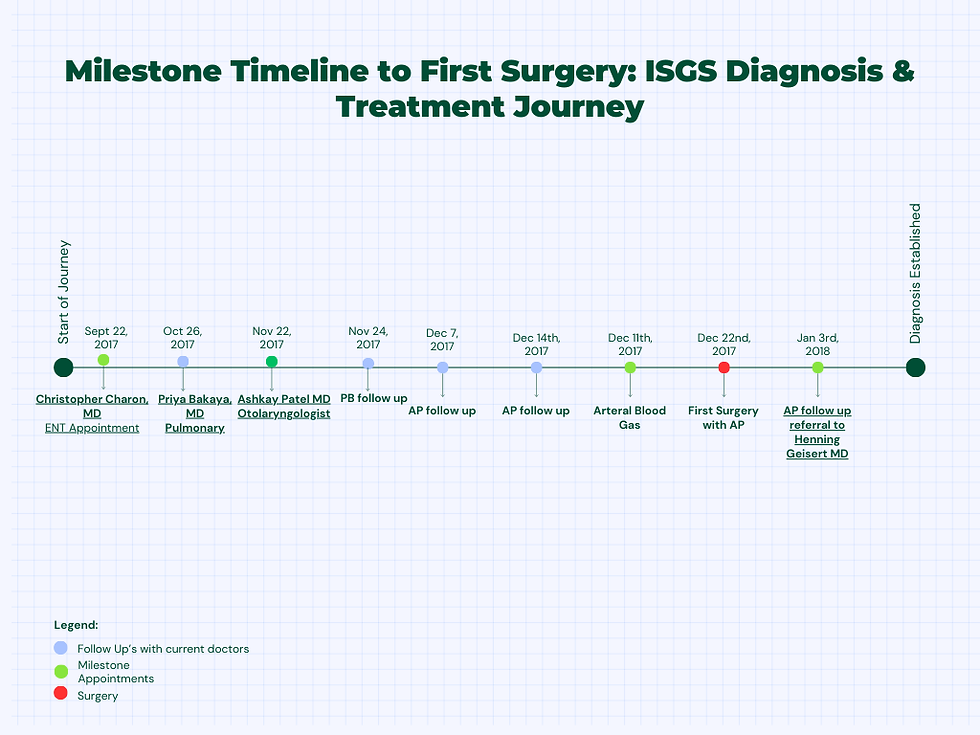
Below is a visual timeline of procedures from my first symptoms to first surgery, followed by ongoing treatments. These include balloon dilations, biopsies, and steroid injections that have helped manage my airway narrowing.
📋 Full Procedure Log
2017
• December – Dilation with Balloon
2019
• February – Dilation with Balloon and Biopsy
2020
• May – Dilation with Balloon and Steroid Injection
• July 8 – Steroid Injection
• July 29 – Steroid Injection
• August 18 – Steroid Injection
• September 9 – Steroid Injection
• November 18 – Steroid Injection
2021
• January 20 – Steroid Injection
• May 18 – Steroid Injection
• August 26 – Steroid Injection
• September 15 – Steroid Injection
• December 7 – Steroid Injection
2022
• April 27 – Steroid Injection
• May 27 – Steroid Injection
• August 5 – Steroid Injection
• December 14 – Steroid Injection
2023
• January 3 – Steroid Injection
2024
• October – In-Office Dilation
2025
• February – Dilation with Balloon
💔 The Emotional Impact
Hearing the words “You have iSGS” felt like being dropped into completely unfamiliar territory. Idiopathic Subglottic Stenosis? Like, what even is that? What does idiopathic mean? At just 24 years old , healthy, driven, and newly stepping into adulthood, I never expected to be facing a rare airway disease that has no clear cause and no guaranteed fix.
In some ways, I was relieved. It was validating to know that what I had been feeling wasn’t just in my head , there was something going on. But that validation came hand-in-hand with a heavy emotional toll. I felt frustrated, sad, and honestly, scared. I had no roadmap. Just a diagnosis that raised even more questions.
The emotional toll wasn’t mine alone, my family felt it too. My now-husband had already been urging me to seek answers for months. Now, we both had to accept that this diagnosis would be something we’d live with and manage together.
Even after the label of iSGS was finally placed, it didn’t feel like much had changed. It was still idiopathic. Still unexplained. Doctors had theories, maybe mold exposure, vaccine reaction, chronic stress, even endometriosis. But none of them could tell me for sure. Every biopsy just came back the same: inflammation. That’s all. And that ambiguity can be exhausting.
Despite that, I was never alone. My husband was there for every surgery, sitting in waiting rooms, waiting to hear how it went. He tried to come to every in-office steroid injection, but COVID restrictions meant he sometimes had to stay behind. When I needed support the most, he showed up.
Before surgeries, my body would scream for help, I’d get headaches and dizziness, especially after working out (which used to be my stress relief). Recovery usually took about 1–3 days, but when you’re also breastfeeding or chasing after a toddler, healing isn’t linear. It’s slower, messier, and heavier.
Still, with support and time, I’ve learned how to live with iSGS, and to speak up for myself, even when the answers aren't clear.
🩺 What the Doctors Told Me
Idiopathic Subglottic Stenosis, even the name sounds like a riddle. The more I learned, the more I realized: this is a rare and largely misunderstood condition. iSGS is a diagnosis of exclusion, which means they had to rule out everything else first, autoimmune disease, tumors, trauma, infections, before landing on… well, the unknown. Idiopathic quite literally means: "we don’t know the cause."
I was told there is no known trigger, no proven way to prevent it, and most importantly, no cure.
I received my formal diagnosis from Dr. Henning Geisert, and from there, I was referred to specialists who would become a crucial part of my long-term care. I worked with Dr. Zachary Wallace (rheumatologist) to rule out systemic autoimmune diseases. I underwent extensive bloodwork, testing, and even tried Rituximab infusions, two five-hour sessions, to lower inflammation markers like my C-reactive protein. The infusions didn’t seem to make a significant difference, but it was part of the journey to rule out other causes.
Eventually, I transitioned fully under the care of Dr. Ramon Franco, an otolaryngologist, who has since been my main point of care.
The plan from that point forward was focused on airway management, and included:
Balloon dilations to physically widen the narrowed area in my airway
Steroid injections to reduce inflammation and prolong the time between surgeries
Regular scopes and spirometry to monitor airway function
Biopsies, especially when symptoms flared, though these often came back with vague findings, usually just “inflammatory tissue”
Over time, this process became a routine, albeit one I never asked for. I had to learn how to read my body, anticipate my symptoms, and advocate for the right timing of my interventions.
Even though I have a “diagnosis,” it often feels like a placeholder, an umbrella term for something science hasn’t quite figured out yet. I still don’t know what caused this. It could have been mold exposure, vaccine injury, chronic stress, endometriosis, radioactive iodide from zapping my thyroid, the MTHFR mutation, or maybe something no one has thought of yet. And that’s a strange thing to carry, knowing you’re managing something real, something measurable, yet still… a mystery.
🗣️ Looking Ahead
Receiving this diagnosis marked a shift, from total uncertainty to having some understanding. It didn’t give me all the answers, but it gave me a name, a path forward, and the realization that self-advocacy is everything. If I hadn’t pushed for more testing after that first scope, I might still be searching.
In upcoming posts, I’ll walk you through my full treatment timeline, share what I’ve learned about living with a rare disease, and reflect on how I’ve found strength through knowledge, persistence, and community.
And if you’re navigating something similar, please know: your voice matters, even when your airway tries to take it from you.
Alright, lastly, my biggest advice is to question everything, from everyone, including your doctors. Always stay research-minded but cautious, because you only have one life and one body. If the voice in your head is saying, “Hmm, I don’t know about this,” always listen. We never truly know how a medication or treatment will affect us personally.
Please also keep in mind to always find out if you have the MTHFR gene mutation and which copies you carry. This is extremely important because it affects your body's ability to detox naturally, and depending on your specific copies, your detox rate can be significantly reduced. Unfortunately, many doctors don’t consider the MTHFR mutation a big deal, but it is, there’s just very little research on it, even though it’s expected that about 60% of the population has it.
💡 Keep in mind: there is a growing body of research into iSGS, and new treatments are on the horizon, including trials with GLP-1 medications and other immune-modulating therapies. Hope is real, and progress is happening.
If you're interested in a detailed breakdown of appointments, procedures, and insights from each stage, I’m happy to share that too, just let me know.



